The COVID-19 infection, termed a pandemic by WHO, has as on 14th April, 2020 spread to more than 197 countries. Life is getting disrupted not primarily because of the mortality or morbidity caused by the virus but more as a consequence of the massive global measures already initiated to contain the rapid spread of the virus. Global economy is taking a beating never seen before. Technology plays a critical role in the management of COVID-19 infection. This includes teleconsultations, promoting customised Health Literacy- the eWay, genome sequencing, drug development, interactive real time maps for monitoring and use of robots and drones1.
COVID-19, or the Corona Virus, has in a few weeks transformed life on this normally peaceful planet. This exponential disruption is not primarily because of the mortality or morbidity of the virus itself, but is a consequence of the massive global measures sought to be taken, to contain the possible rapid spread of the virus. Response has to be almost in real time. Global economy itself is taking a beating never seen before. Is this just the beginning or is the worst over. What is the role of technology in management of COVID-19? Let us have a look.

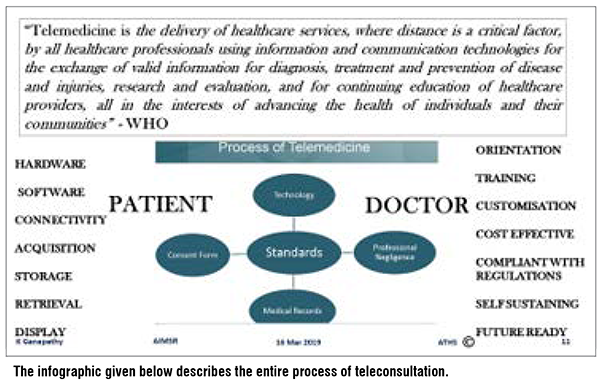
Telehealth can considerably increase access to specific care. Telemedicine can be useful to evaluate and reassure patients remotely, to help decide who needs to be seen in a hospital OP or ER. Diagnosing coronavirus-like illness (CLI) on a clinical basis can be confidently done virtually, without laboratory tests. Treatment monitoring and reviews can be done with the ‘patient’ self-quarantined at home. Care would be commensurate with acuity and nature of the symptoms. This helps with infection prevention and control. Elderly. or others with other increased susceptibility to CLI, run an additional risk of being susceptible to further illnesses in a hospital environment, Through telemedicine, if admission is deemed to be required, it can be made directly into an isolation ward bypassing the casualty. This simple step in itself would reduce risk of the virus spreading.
A major possible concern is the flooding of healthcare centres and hospitals for unnecessary examinations and reassurance. This would not only increase the risk faced by healthcare providers, but also reduce the quality of treatment required for those who do need it. In a potential pandemic setting, increased attention must be paid to the health of the healthcare providers (HCP). Tele evaluation enables even quarantined HCP’s to work from their own homes, significantly increasing their safety and bolstering the workforce to respond to a crisis. When patients are seen in their own homes, providers and health systems will be able to triage and screen many more patients than in face to face encounters.
Patients could also have other healthcare needs unrelated to coronavirus. Some will be afraid to go to a healthcare facility for fear of catching the epidemic. Telehealth could be the answer. Symptom trackers and chat bots is another promising area for virtual management of suspected coronavirus infection. These technologies allow algorithms to be created and continually modified as more is learnt. Dedicated customised bots can even interact with patients, performing assessments, triage and provide ongoing support. The bots can escalate an interaction to a telehealth encounter or refer the patient for in-person care. It is simple to develop a user friendly customised even region-specific software. Detailed travel and exposure histories can be obtained.
Providers must know and understand their role in this as in any other healthcare crisis. They should be well informed and trained to follow national or World Health Organization (WHO) guidelines. They should understand that telehealth is a powerful tool in fighting this outbreak. Telehealth virtual visits are typically sufficient to complete a robust initial assessment. This allows the provider to assign a risk category or make other diagnoses. Some patients may require additional care, as certain medical peripherals may not be available at home for serial monitoring. A high-risk patient may need to be tested outside of home. Escalation of care may be required.
Reimbursement in a non governmental setting needs to be addressed. Ideally health insurance companies should reimburse teleconsultations. From an RoI (Return on Investment) perspective, it is in the interest of insurance companies to promote earlier diagnosis to prevent avoidable hospitalisation later. One key advantage of telehealth is speed. Patients can access clinicians 24/7 without an appointment or physical trip to the doctor. Crisis management should include the Government of India and state governments unambiguously laying down clear rules for legalising teleconsults.
The US Congress last week legalised telehealth for coronavirus screening. The American Telemedicine Association has applauded the sanction of 500 million US$ exclusively for telehealth from the $8 billion emergency funding legislation, to expand the toolkits of healthcare professionals working to combat the COVID-19 outbreak. This was possible only because of intensive lobbying by the ATA and the political will exhibited by Democrats and Republicans alike. Will this followed in other countries?
Both the Center for Disease Control in the USA and WHO have recommended using telemedicine, to direct patients to the right site of care during the outbreak. This would also considerably minimise the use of personal protective equipment, such as gloves and masks, by healthcare providers. The economic benefit of this very doable procedure is staggering.
1. Clinical examination from a distance: Digital technology can make distance meaningless Geography today is history! The healthcare provider can virtually appear in all offices where there are video conferencing systems, PC’s and laptops. Even an entry-level smart phone will suffice. Sophisticated tele triage can be done. Detailed travel and exposure histories can be obtained. Automated screening algorithms can be developed and local epidemiological information can be used to standardise screening and practice patterns across different providers in different geographies. A reasonably adequate clinical examination can be done remotely. All that is required is dependable band width and good inexpensive video software. Fever, cough and shortness of breath can all be evaluated from a distance. A bright torch at the remote end can be used to illuminate the throat and nose of a suspected contact. This can clearly be seen by the healthcare provider wherever he/she is. Digital sounds and heart sounds. The audio file can even have a description of the sounds with a provisional diagnosis which the clinician at the other end can confirm. Blood pressure, pulse rate, respiratory rate, oxygen saturation, and temperature can also be monitored remotely.
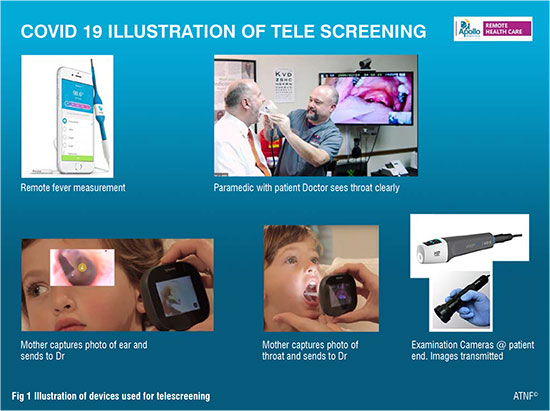
Though not relevant in mass screening, if specifically indicated a patient friendly 6-lead, FDA-cleared, medical grade, bluetooth enabled pocket electrocardiogram (ECG) device can be used even without a paramedic. The automated diagnosis which comes along with the ECG tracing can be sent to a physician through an ordinary smart phone Similar 12 lead ECG will soon be available. A pocket ultrasound device can be attached to a smart phone to give real-time, high-resolution ultrasound images, similar to what one sees with a traditional ultrasound in a radiology department (not relevant here just to let the reader know what is available in the market today). State-of-the-art medical care goes to where it is needed not vice versa . An ENT expert can peer into the ear and an ophthalmologist into the eye with the patient several thousand miles away. A computergenerated report with the doctor’s digital signature with annotated colour images can reach the patient’s smart phone with an ePrescription in a few minutes. This transaction is stored in the cloud for perpetuity. Telemedicine today cannot take a swab of the throat to collect a sample for scientific testing. However theoretically a robot can even do this in the not too distant future.
2. Promoting health literacy the eWay: Today in India, we hear an audio message preceded by a cough every time we make a telephone call. Similarly, a very short video can be sent to a billion mobile phones. Promoting visually aided diseasespecific health literacy will go a long way to create much needed awareness. While WhatsApp no doubt has created awareness never before done in the history of humankind, it also gives room for spreading misinformation and disinformation. This is leading to fear psychosis and avoidable panic.
3. Artificial intelligence: Developing AI algorithms will help identify patterns using Big Data analysis. This will help predict outbreaks before they actually occur. Meticulous follow up of every contact with an afflicted patient will help develop preventive and therapeutic measures.

4. A doctor in your pocket: Medical devices can be added on to a smart phone. Eventually a swab sample can be collected in a smart device and connected to a smart phone with optical scanning facilities. The COVID-19 pandemic will no doubt reduce the time taken from ‘bench to bed’.
5. Genome sequencing of the virus RNA was done within a record time of four weeks, whereas it took several months for sequencing the SARS virus. One is increasingly becoming painfully aware that in spite of uniform standards and protocols personalised medicine may be necessary for a specific individual. Response to standard medication may depend on your genes. Genome sequencing may in the future address these concerns. Laboratories world wide are racing to make available a vaccine for the COVID-19. Super computers and even quantum computing may be used.
6. Drug development: A cure for COVID-19 infection is required yesterday. In silico trials will be used. In these trials an individualised computer simulation is used in the development or regulatory evaluation of the medicinal product. While completely simulated clinical trials are not feasible with current technology and understanding of biology, its development would be expected to have major benefits over current long drawn clinical trials. ‘Virtual’ patients would be given a ‘virtual’ treatment, enabling observation through a computer simulation of how the drug performs and whether it produces the intended effect, without inducing adverse effects. Such in silico clinical trials would significantly could help to reduce, refine, and partially replace real clinical trials for COVID-19 management. Nanoparticles could operate as precise drug delivery systems.
7. Interactive maps for monitoring: Data is instantaneously updated in real-time through online dashboards available globally. This is totally downloadable in the public domain. Organisations and governments have come together like never before. Tens of thousands of data scientists and scientists from every possible discipline are making use of futuristic technology to contain the Corona virus.
8. Robots: Wuhan started using robots in quarantined wards immediately after the outbreak. Robots are now routinely used in many hospitals in China and in other countries. This certainly reduces risks of paramedics, nurses, and doctors catching the infection. A recent news in the media mentioned China opening a hospital entirely staffed by robots. The facility, dubbed the Smart Field Hospital, carried out basic screening tasks such as tracking temperature, heart rate and blood oxygen levels, with robots. Other robots tended to patients by bringing them food and drink, as well as medicine. Some robots put on a little dance to keep patients entertained. A team of researchers even successfully demonstrated a robot that can swab patients’ throats remotely, minimising contact for healthcare workers at the hospital.

9. Drones can be deployed to drop essential supplies medical and non-medical items to quarantined groups. Spain, Kuwait, and United Arab Emirates, drones equipped with loudspeakers have been telling roaming citizens to go back to their homes. Agricultural models have been modified to spray disinfectant on public areas, and drones have also transported medical and quarantine supplies to reduce people’s exposure to each other and reduce delivery time.

Conclusion:
Digital health is bringing about a real revolution, shifting the point-of-care to where it should have been all this time - the patient’s abode – not a hospital. Policymakers should provide incentives for healthcare facilities and physicians to use telemedicine and technology-enabled remote care in their normal healthcare practice. Awareness must be raised among patients about the benefits of telehealth. Technology acceptance as a behaviour modification strategy should be considered. Even in the USA 88 per cent of companies with 500 or more employees offered telemedicine as part of their health benefits last year. Only 9 per cent of eligible employees used it. Deploying TECHNOLOGY on a war footing is the only way we can contain this pandemic. However, let us never ever forget that technology is a means to an end not an end by itself. Hitherto septuagenarians like me belonging to the BC era somehow felt that technology was developing solutions first and then searching for problems where they could be used. The COVID-19 pandemic offers an urgent genuine reason why we should use technology not tomorrow not today but yesterday. Hopefully this global crisis will result in the right mix of deploying technology and TLC (Tender Loving Care) for the benefit of our fellow brethren.

Addendum: On March 25th 2020 the Ministry of Health Govt of India notified an amendment to the Medical Council of India Act. Telemedicine Practice Guidelines have been elaborated. The Prime Minister India has repeatedly exhorted Indian citizens to start using Telemedicine. The last 6 weeks have witnessed an unprecedented interest, growth and development of Telehealth in India. The Telemedicine Society of India has been given the mandate of sensitizing 500,000 doctors to the use of telehealth. Proof of concept trials have just started. Telehealth in India will now be divided into the BC and AC era ( Before Corona / After Corona) era!
References:
1, Also see Youtube presentation https://www.youtube.com/watch?v=7lmJ6ByIoEY&feature=youtu.be Deployment of Telehealth in COVID19